Health care costs too much. The cost of care threatens Kaiser Permanente’s social mission to provide affordable, quality health care to all.
There are no simple solutions, but KP has many advantages that others do not—including our integrated model of care that can better manage and prevent illness; a prepaid, nonprofit structure that keeps revenue in the system to better serve members and patients; and unit-based teams. As they create the best place to work, UBTs are continuously improving quality, service and affordability at the front lines of care.
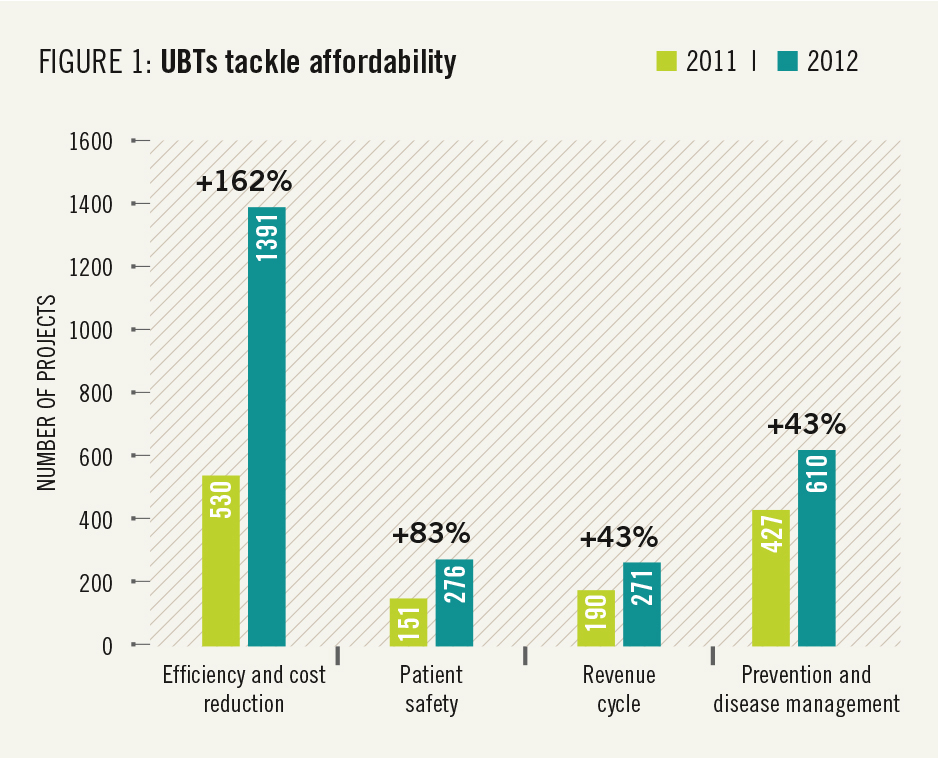 This report highlights many ways that unit-based teams are getting results that matter to members and patients. Affordability of care, one of the issues that matters most to members, was the fastest-growing focus area for UBTs in 2012 (see Figure 1).
This report highlights many ways that unit-based teams are getting results that matter to members and patients. Affordability of care, one of the issues that matters most to members, was the fastest-growing focus area for UBTs in 2012 (see Figure 1).
Teams launched nearly 1,400 efficiency and cost-reduction projects last year, more than doubling the number of such projects undertaken in 2011.
That bodes well for the future, because the number and effectiveness of UBTs’ performance improvement projects increase as teams develop. For instance, UBTs that are rated high performing—defined as reaching Level 4 or 5 on the UBT Path to Performance—are three times more likely than Level 1 teams to take on cost-reduction projects, using proven tools such as process mapping, the “6S” performance improvement tool, and spaghetti diagrams (see Figure 2).
 And these teams are getting results. Waste- and cost-reduction projects can yield immediate savings of $20,000 to $50,000. Spread across the organizations, these efforts could save more than $100 milliion a year. Some examples of the work being done:
And these teams are getting results. Waste- and cost-reduction projects can yield immediate savings of $20,000 to $50,000. Spread across the organizations, these efforts could save more than $100 milliion a year. Some examples of the work being done:
- At the Baldwin Park Medical Center Laboratory in Southern California, phlebotomists worked to reduce the use of more expensive butterfly needles, substituting standard needles when they will work—saving more than $45,000 in 2012. Other labs are also doing this; potential savings if implemented program-wide: $2 million.
- The Fremont Medical Center Operating Room team in Northern California, after taking business literacy training and looking at their own costs and budget, identified wasteful practices in the use of ready-made surgical supply packs, saving about $34,000 a year. Potential savings if implemented program-wide: $750,000.
- The Point Loma Primary Care team at the San Diego Medical Center in Southern California applied 6S to organize supplies and standardize ordering, saving more than $20,000 in 2012. Potential savings if implemented program-wide: $4.2 million.
As these examples show, individual teams can implement improvements that can save a significant amount of money in their own corner of the system. As practices spread among the 3,500 unit-based teams now working across Kaiser Permanente, the savings can add up quickly.
Achieving the full cost-saving potential of UBTs will not be automatic. More teams need to take on cost and waste issues. Even with the jump last year, only one-fifth of UBTs undertook such projects. Successful practices must be spread more systematically across departments, facilities and regions. And more teams need the kind of business training that led the Fremont OR team to act.
 But those changes are coming. “The growing number of cost saving and efficiency projects are helping build a culture of savings and waste reduction among high-performing teams across KP,” says Peter Nixon, director of metrics and analytics, Office of Labor Management Partnership.
But those changes are coming. “The growing number of cost saving and efficiency projects are helping build a culture of savings and waste reduction among high-performing teams across KP,” says Peter Nixon, director of metrics and analytics, Office of Labor Management Partnership.
High-performing UBTs outscored others on two questions in the 2012 People Pulse survey regarding employee views of their department’s efficiency. (see Figure 3). Members of high-performing teams are more likely to say their departments have efficient work procedures and seek improvements to reduce costs.
“These findings suggest that members of high-performing teams see waste reduction and efficient work processes as part of their job,” Nixon says. “That is good news, because it’s the discretionary effort, commitment and intelligence of frontline teams that gets results.”

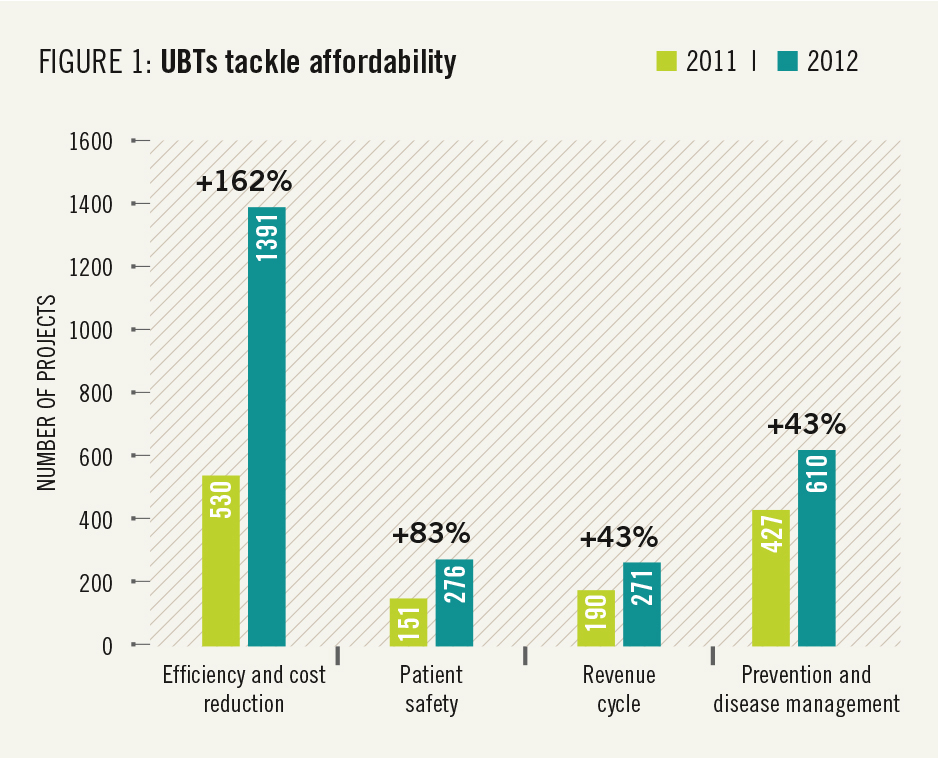 This report highlights many ways that unit-based teams are getting results that matter to members and patients. Affordability of care, one of the issues that matters most to members, was the fastest-growing focus area for UBTs in 2012 (see Figure 1).
This report highlights many ways that unit-based teams are getting results that matter to members and patients. Affordability of care, one of the issues that matters most to members, was the fastest-growing focus area for UBTs in 2012 (see Figure 1). And these teams are getting results. Waste- and cost-reduction projects can yield immediate savings of $20,000 to $50,000. Spread across the organizations, these efforts could save more than $100 milliion a year. Some examples of the work being done:
And these teams are getting results. Waste- and cost-reduction projects can yield immediate savings of $20,000 to $50,000. Spread across the organizations, these efforts could save more than $100 milliion a year. Some examples of the work being done: But those changes are coming. “The growing number of cost saving and efficiency projects are helping build a culture of savings and waste reduction among high-performing teams across KP,” says Peter Nixon, director of metrics and analytics, Office of Labor Management Partnership.
But those changes are coming. “The growing number of cost saving and efficiency projects are helping build a culture of savings and waste reduction among high-performing teams across KP,” says Peter Nixon, director of metrics and analytics, Office of Labor Management Partnership.