An Internal Medicine team in Ohio improved its workflow and increased from 62 percent to 74 percent the number of diabetes patients with cholesterol levels under control—surpassing the region’s goal—even while coping with a staff shortage.
A medical/surgical unit at Fontana Medical Center, in Southern California, went 23 consecutive months without an incidence of hospital-acquired pressure ulcers—after previously experiencing seven to 10 cases a year.
Colorado’s regional laboratory improved the accuracy of its transfer and tracking records from 90 percent to 98 percent, significantly reducing rework and speeding turnaround times for patients’ lab results.
These outcomes, and hundreds of others across Kaiser Permanente, were the result of performance-improvement projects undertaken by unit-based teams (UBTs)—Kaiser Permanente’s strategy for frontline engagement and collaboration.
Physician involvement in UBTs to date has varied, and generally remains limited. However, based on evidence from across Kaiser Permanente, we believe unit-based teams can help physicians achieve their clinical goals and improve their efficiency and deserve their broader involvement.
How UBTs work
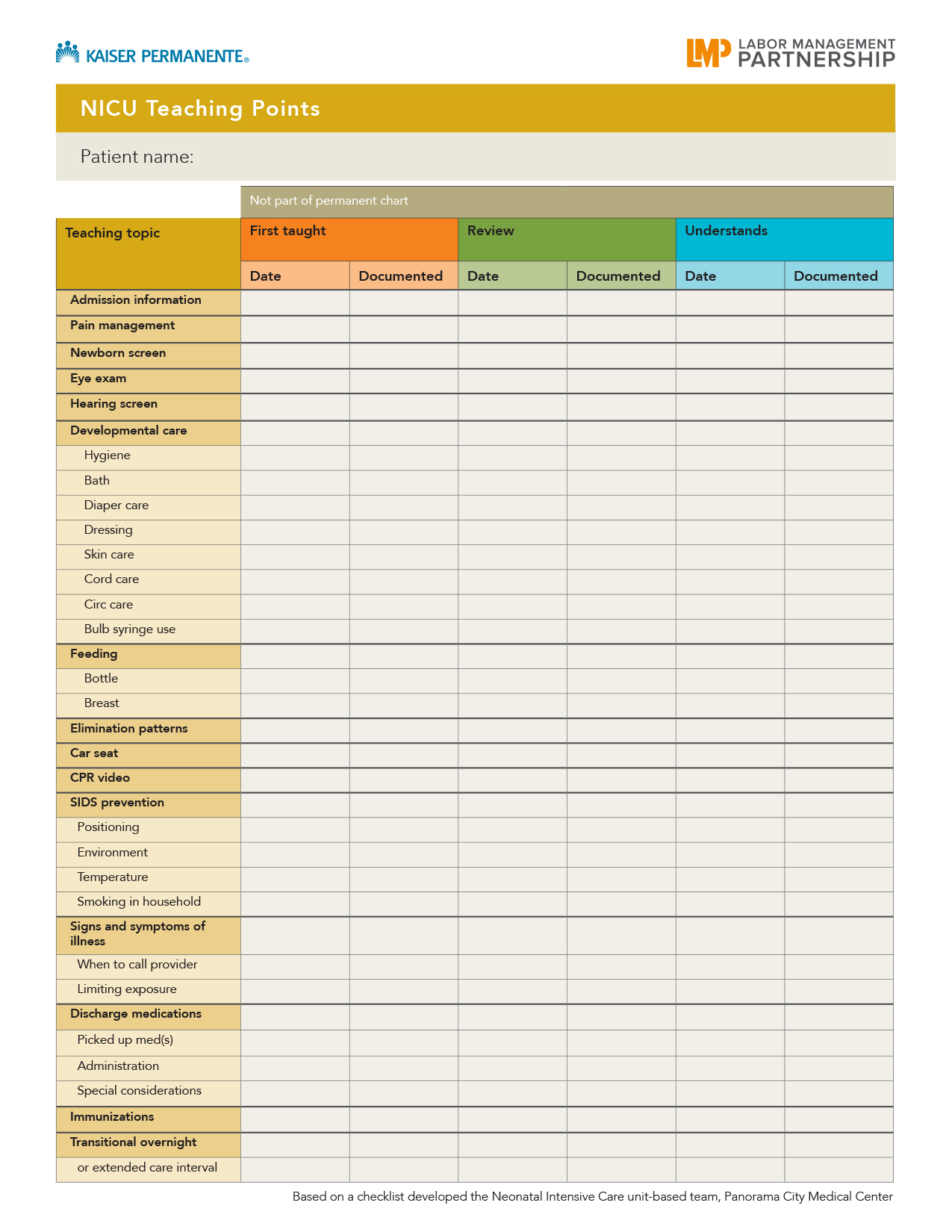
Teams identify performance gaps and opportunities within their purview—issues they can address in the course of the day-to-day work, such as workflow or process improvement. By focusing on clear, agreed-upon goals, UBTs encourage greater accountability and allow team members to work up to their scope of practice or job description. Achieving agreed-upon goals, in turn, promotes continuous learning, productive interaction, and the capacity to lead further meaningful change.
As a strategy for process and quality improvement, UBTs draw on the study of “clinical microsystems” by Dartmouth-Hitchcock Medical Center and the Institute for Healthcare Improvement. “If we want to optimize a system, it's going to be around teams and teamwork, and it's going to cut across hierarchies and professional norms,” says Donald Berwick, MD, president and CEO of IHI and President’s Obama’s nominee to head the Centers for Medicare and Medicaid Services. “Unit-based teams and much better relationships between those who organize systems and those who work in the systems are going to be essential.”
Four kinds of benefits
The focused nature of UBT activities translates to four broad benefits to physicians and patients:
- Clinical benefits: Saving lives and improving health
- Operational benefits: Using resources wisely and improving efficiency
- Member/Patient benefits: Giving a great patient-care experience
- Physician/team benefits: Improving team performance and worklife
The example below, of a positive clinical outcome in one unit, shows how UBTs use practical, frontline perspective to solve problems.
Simple solutions get results
The Internal Medicine department at Hill Road Medical Offices in Ventura (SCAL) faced a practical challenge: Patients with an initial elevated blood pressure reading need to be retested after waiting at least two minutes—but they often left the office before the staff could do a second test. In fact, the staff was doing needed second checks only 26 percent of the time as of March 2008.
The team’s simple solution: A bright yellow sign reading, “Caution: Second blood pressure reading is required on this patient,” which employees hang on the exam room door so the physician or staff would be sure to do the test.“The teams come up with good ideas about workflow because these are the folks in the trenches and they see the headaches,” says Prakash Patel, MD. “They share ideas and work out processes that help.”
In just one month, the department’s score on giving second blood pressure tests was 100 percent. Their score on the regional clinical goal of hypertension control went from 76 percent in August 2008 to 79.8 in May 2009, just below the regional goal of 80.1 percent.
"I strongly encourage all chiefs of service to champion the unit-based team in their department by either active participation or as a physician advisor, particularly regarding quality, service and access initiatives," says Virginia L Ambrosini, MD, assistant executive medical director, Permanente Human Resources.
UBTs are taking hold at the right moment for Kaiser Permanente. At a time when health care providers are under pressure to contain costs, maintain quality, and improve service, UBTs have the problem-solving tools to address those issues.
Read the full article, including principles of employee engagement and tips for selecting a performance improvement project.