Southern California
Help Video
How to Find UBT Basics on the LMP Website
LMP Website Overview
How to Find How-To Guides
This short animated video explains how to find and use our powerful how-to guides
How to Find and Use Team-Tested Practices
Does your team want to improve service? Or clinical quality? If you don't know where to start, check out the team-tested practices on the LMP website. This short video shows you how.
How to Use the Search Function on the LMP Website
Having trouble using the search function? Check out this short video to help you search like a pro!
How to Find the Tools on the LMP Website
Need to find a checklist, template or puzzle? Don't know where to start? Check out this short video to find the tools you need on the LMP website with just a few clicks.
Videos
Redefining What's Possible
(3:26)
Medical Assistant Sandra Da Rocha shares how she overcame her fear of taking college-level courses—and of using a computer—and signed up for online courses available to union-represented employees through the Ben Hudnall Memorial Trust.
TOOLS
Poster: No One Walks Alone
Format:
PDF (color and black and white)
Size:
8.5” x 11”
Intended audience:
Frontline employees, managers and physicians
Best used:
Learn tips from a Southern California team that has drastically reduced patient falls.
Deck: How UBT supporters are helping teams sort out competing priorities and demands
Improve service scores. Reduce waste. Retain members. Gain new members. Cut wait times. Work safer. Perfect patient safety. Innovate care.
Teams are juggling constantly, trying to meet their own objectives, move forward on initiatives related to facility, regional and national goals, and comply with regulatory requirements—all in a competitive economic environment.
When the curve ball comes sliding in, it can be one thing too many, derailing a strong team or keeping a struggling team at ground level. So a host of unit-based team supporters are turning their attention to strategies to help unit-based teams prioritize competing demands—from personalized mentoring to intensive workshops for co-leads.
“I see my role as taking away the noise and the chaos…to help them figure out, ‘Realistically, how many things can we work on at once?’” says Denise Johnson, San Jose Medical Center continuum of care administrator and a UBT sponsor. “I have to help them not be crazy, because we don’t want a lot of projects that don’t make a difference.”
Here are four strategies for helping teams.
Strategy #1: Planning pays off
Every year, labor and management sponsors at the San Jose Medical Center sit down with their UBT co-leads to develop an operating plan. The plan flows from Kaiser Permanente’s organizational goals as well as from regional goals, facility priorities, and the needs of the department. Each sit-down includes the service area’s UBT consultant and its union partnership representative. Projects emerge naturally from that plan, with teams turning to the Value Compass and a tool called a PICK chart to fine-tune their priorities.
“They have to figure out what’s in their sphere of influence,” says Eric Abbott, the area’s union partnership representative. “What are the things they can change, and of those things, how much time do they have?”
When Johnson became sponsor of one San Jose team, it was immediately clear to her the UBT had too much on its plate. She worked with the team to winnow eight projects down to two.
“In my experience, people get bogged down with the to-do list and sometimes don’t stop and think about what’s really on that list and what effort does it serve,” she says. “They thought I was crazy. They came from a mentality where ‘more is better.’”
Strategy #2: Urgency can be a tool
Two years ago, San Diego’s interventional anesthesia unit-based team was humming along in its performance improvement work when it got hit with the news that co-pays for patients who suffer from chronic pain would be increasing sharply.
The 14-member team responded with a new service project, a multiphase communication plan to help members understand the new co-pay and their options. And then the next wave broke: The team learned it had a matter of days to move into a new specialty services building. It suspended the co-pay project to plan for and complete the move.
One key performance improvement tool—a process map—proved instrumental. The team created a detailed map that laid out every piece of work that needed to be done in preparation for the transition, from changing procedures to adapting to a new phone system to altering workflows based on the new floor plan.
“They simply became a single-issue team,” says their UBT consultant, Sylvia Wallace, of the 2011 move.
With the process map in hand, the team spotted an opportunity to weave communication about the new co-pays together with communication about the move. As a result, it didn’t miss a beat in providing its members with critical information about available financial assistance.
The comprehensive plan helped the unit’s service scores hold steady through the transition—and then increase at the new facility. The moving plan became a template for other departments, which are still moving into the Garfield Specialty Center.
“Everyone participated. All types of ideas were solicited and implemented,” says Grace Francisco, the assistant department administrator and the management co-lead at the time. “Everyone has a role and accountability for each step.”
Strategy #3: Take time to train
Teams stand a better chance of weathering competing demands when they have a solid understanding of partnership principles and processes as well as performance improvement tools and methods.
In Colorado, the UBT consultants used LMP Innovation grant funds to host a two-day workshop centered on two regional priorities. Co-lead pairs from throughout the region learned how best to serve new members and improve the affordability of KP care by reducing waste and inefficient practices. They walked away with a variety of team improvement tools and resources.
“We are trying to set the teams up to be successful by giving them the time to focus on topics that could have a huge impact in the region in the next few years,” says Linda Focht, a UBT consultant and UFCW Local 7 member.
In San Diego, regular UBT summits bring co-leads together for intensive sessions on given topics. Service area and local union leaders play a major role in structuring the agenda, so the team development matches up with high-level strategy. The joint planning creates a full picture, one that resonates better at the front line and sets up teams to work on projects that make a difference to KP’s reputation.
“Leaders see a lot more than what we see,” says Jenny Button, director of Business Strategy and Performance Improvement in San Diego. “Leaders see what is going on with the competition. They see across all of the different metrics we are working toward. They see at a broad level where our biggest gaps are.”
Strategy #4: One-on-one attention counts
At San Jose Medical Center, sponsors like Johnson and Hollie Parker-Winzenread, an assistant medical group administrator, are coaching UBTs one on one in performance improvement tools to help them set priorities.
“Teams like to jump to the solution,” says Parker-Winzenread. “But they struggle with the process….The gain falls apart, because the process is not strong.”
San Jose’s clinical laboratory UBT is a success story, jumping from a Level 1 to a Level 4 in less than a year after new co-leads worked together to reach joint agreement on the department’s priorities. The team started with tests of change that made strides in attendance. Today, it has moved on to complex projects that require shifting schedules to accommodate demands for getting lab results earlier in the day.
Guidance from their sponsors has helped keep team members on track.
“We’d come up with all of these ideas and projects, and they made suggestions and really helped prioritize what we worked on so we didn’t bite off more than we could chew,” says Antoinette Sandez, a phlebotomist, the team’s union co-lead and an SEIU UHW member.
“You have to help teams to believe in the process,” Johnson says. “As a sponsor I can’t rush the process and say harder, faster, move, move, move. That won’t get us what we want in the long run. Because we’re looking for sustainability.”

Deck: A pilot project spreads hospital-wide to prevent patient falls
Among the telemetry units at San Diego Medical Center, 5 West had a bad reputation: It consistently had the most patient falls at the hospital. In 2011, for example, it had twice as many as the next-worst unit. Patients were suffering, as was morale. Managers and employees tried all sorts of measures to prevent falls—such as posting pictures of falling leaves on patient doors and using color-coded arm bands on patients to indicate fall risk—but nothing was improving patient safety enough.
Only when the unit-based team launched its “No One Walks Alone” campaign in 2012 did the numbers budge. It’s part of a larger trend in health care to shift from trying to assess a patient’s risk of falling to simply treating every patient as a fall risk and ensuring each patient is accompanied—especially to and from the bathroom, which is when most falls occur.
“This is for everybody, not just some,” says Lucila Gonzalez, RN, a UNAC/UHCP member who serves on the UBT’s representative group. After all, patients newly hospitalized after a stroke suddenly cannot do many things they used to do on their own. And elderly patients who were independent at home might resist getting help. “It takes time to adjust,” says Gonzalez.
Spread what works
The pilot project on 5 West—part of a collaboration with the Joint Commission for Transforming Healthcare that also involves six non-Kaiser hospitals—included installing bed alarms to let staff know when a patient was trying to sit up, so a caregiver could dash over and assist. When patient falls decreased dramatically in the first three months of the effort, the practices were spread in November 2012 throughout the hospital. And the results have stood up. The hospital previously had been averaging 16 falls a month. In October 2013, that figure was three a month.
Some employees had doubts about the initiative when it first started, says management co-lead Estela Enriquez. “They said, ‘Just don’t make it cumbersome.’ Others said, ‘It’s just not going to happen.’” Enriquez says, “For me, as a manager, it was an issue of staffing.” At first, it was harder to ensure nurses got their breaks. UBT members worked on their department budget and hired more unit assistants. They also worked together to build in time during the day for their added responsibilities. “We’d see nurses walking around the unit with the patients,” says Enriquez. “Then there was a sense of, ‘OK, maybe we can manage this.’”
The inpatient units are sustaining their results by talking in their huddles about the falls that do happen, rounding on patients hourly to get them out of bed and into the bathroom safely, ensuring that bed alarms are activated and celebrating their successes.
Set ambitious goals
The slogan “no one walks alone,” which came from a UBT meeting, is more than a catchphrase, Enriquez says. “It is one that resonates with patients. The wife of a patient said her husband was embarrassed that ‘a big, strong guy’ couldn’t go to the bathroom by himself. The nurse finally got through to my husband when he said, ‘No one walks alone.’”
Jenny Button, director for business strategy and performance improvement at the hospital, says a key to success is to set an ambitious goal. It’s not enough to work to “reduce” falls or get to four a month, she says. “You have to say, ‘We want no falls.’”
TOOLS
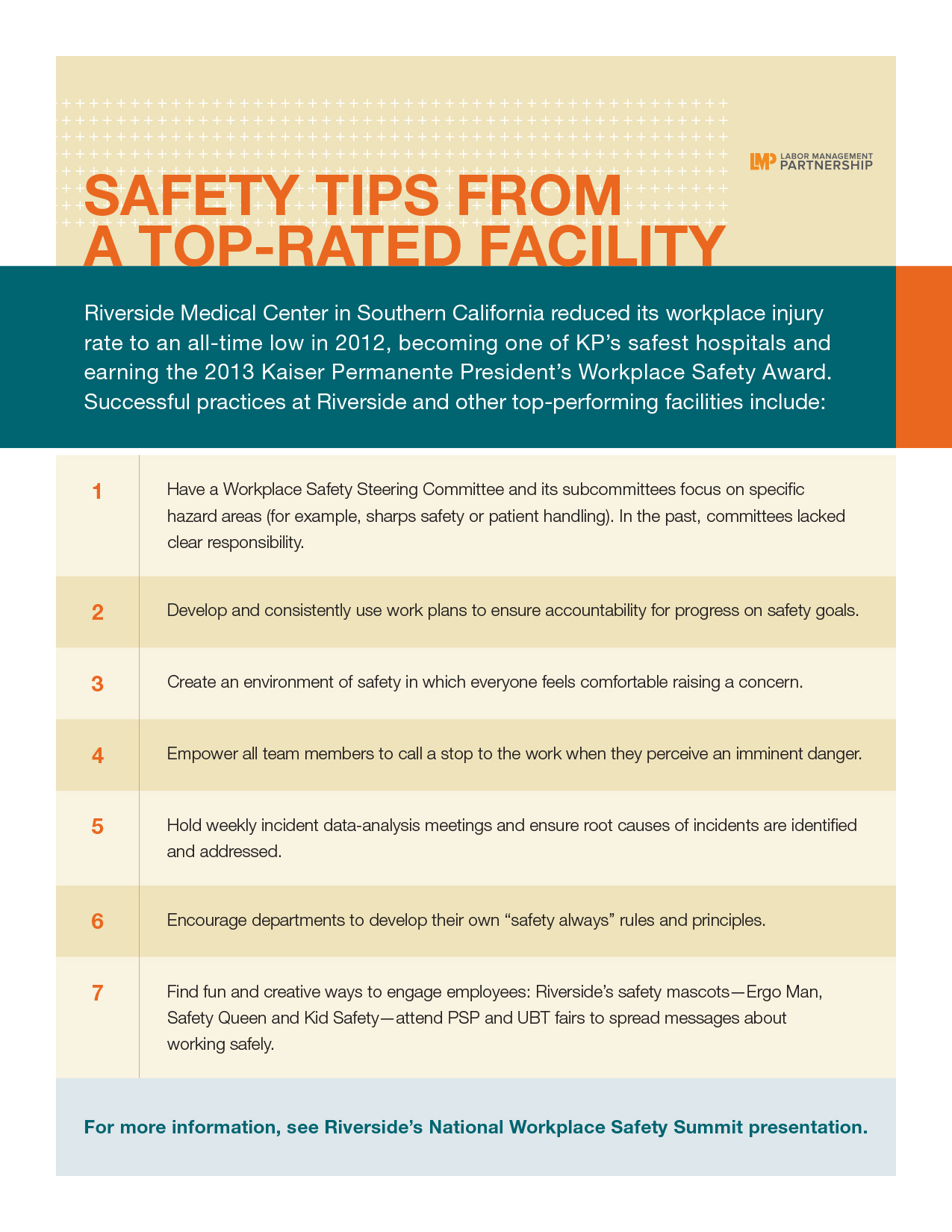
Workplace Safety Tips From a Top-Rated Facility
Format:
PDF
Size:
8.5" x 11"
Intended audience:
Unit-based teams, co-leads, department managers, union stewards and safety leaders
Best used:
Improving workplace safety starts with you. Follow this tipsheet for successful workplace safety practices.
Deck: Team overhauls process to reduce errors
Being accurate 98.9 percent of the time sounds pretty great.
Nearly perfect, in fact, but the Central Sterile Processing department at the West Los Angeles Medical Center sterilizes almost 4,000 trays a month. So even a small percentage has a big effect.
Incorrect trays disturb operating room efficiency. When a nurse or tech has to track down the correct instruments for a surgery, it slows down the OR and increases wait time for patients and their families.
In some cases, inaccurate trays cause surgeries to be rescheduled.
That disrupts patients, who’ve arrived physically and psychologically prepared for an operation, and family members, who juggled their schedules.
It also frustrates doctors and employees. And since many departments are involved in surgeries, the disruptions caused by inaccurate trays creates friction among departments and colleagues.
So, when the UBT brought managers and employees together to review and analyze the department’s data, they had some serious work to do. But the group was able to find errors, spot efficiencies and rearrange workflows.
“The improvement was, in a word, remarkable,” says Marco Bautista, manager, Central Processing.
They worked with vendors to provide pictures of instrument trays and individual instruments to improve the inspection process. They put heavy trays in special sturdy containers to avoid puncturing protective sterile wrapping, and used a buddy system to audit instruments.
The team involved lead techs in daily quality assurance checks on surgery trays, and posted tray accuracy reports and other metrics in the employee break room.
They also held weekly meetings with operating room department administrators, and allowed employees to observe surgical procedures. That helped their understanding of the importance of tray quality and accuracy.
The team hit 99.8 percent a month.
The changes also increased confidence among staff, and created a better working relationship between the Central Processing department and its internal clients.
“We are treated with respect by our peers and others in the hospital,” Bautista says. “The overall image of the department has improved.”
Deck: Active sponsors drive high-performing teams. Can partnership overcome the short supply?
If you ask Los Angeles Medical Center sponsors Ilda Luna and Sanjit Sodhi for the secret to successful sponsorship, they’ll agree it boils down to investment—of time, trust and respect—in each other, in their teams and in the collaborative work process.
Luna, a family medicine receptionist, and Sodhi, the chief financial officer for LAMC, didn’t know each other when they were asked to co-sponsor the Health Information Management, Admitting and Patient Revenue, and the local business office teams—teams that were failing to meet performance goals and were entrenched in mistrust between labor and management.
“Sanjit said, ‘Tell me what I need to do to get us up and running,’ ” recalls Luna, a member of SEIU-UHW. “I said, ‘You need to meet with your teams. If you invest time in labor, you’ll get huge dividends.”
Like most investments, success didn’t happen overnight — and it wasn’t guaranteed. But after a year and a half of perseverance, dedicating time and hard work to supporting the work of those teams, the pair has watched the departments go from being in the red in most metrics to seeing huge improvements in areas like attendance and co-pay collection.
“We’re taking on types of projects that we could never have dreamed of a year ago,” Sodhi says. “And when you work though relationship issues and put the focus back on partnership and performance improvement, it’s highly satisfying.”
What’s so special about sponsors?
A study by Johns Hopkins University, Rutgers University and Kaiser Permanente identified five key characteristics of high-performing teams, including “consistent, aligned and visible sponsorship.” It confirmed what has been seen throughout the organization—strong sponsorship and support from higher levels of leadership are key factors in a team’s success.
The reasons are straightforward. Many frontline workers say simply having leaders’ involvement and support gives their work validation, letting them know that what they’re working on is important, that their contributions matter. In addition:
- Sponsors mentor unit-based teams and connect them with effective practices and other resources to help them do their work.
- They help break down barriers and provide guidance on setting goals that line up with local and national performance goals.
- They act as role models and advocates for working in partnership.
“There are teams that need both management and labor sponsors to model partnership behaviors, who can agree to disagree and who can have some healthy courageous conversations till they get to an outcome,” says Vicki Barkan, the UBT consultant at the Los Angeles Medical Center. “Sometimes teams and co-leads haven’t experienced that, so they need to see it. It really helps to further the team dynamics.”
Sodhi agrees.
“As sponsors,” she says, “we have the same common goals and mutual respect for each other” that team members should have. “It trickles down to the rest of the UBT.”
“Sponsorship is a way to help move UBTs forward,” says Diane Ochoa, the regional director for Medical Group Support Services in Northern California and a former San Jose Medical Center medical group administrator. “It’s just like having a mentor, somebody you can talk to, to help you with issues and celebrate with you, and be there to really acknowledge the work you’re doing.”
So, what’s the problem?
Yet sponsorship is still a developing area in the partnership structure, even though many regions find that without active union and management sponsors, UBTs’ performance improvement work stalls.
Several challenges get in the way, and chief among those is time. Sponsors repeatedly cite the difficulty of finding time in their regular work to mentor teams. Labor sponsors face the added challenge of needing to cover their duties when they’re away from their usual post, lest those duties fall to colleagues.
Even with a commitment from facility and department leadership to backfill her position when her sponsorship work takes her away from her regular job, Luna, who is the union co-lead for the medical center’s LMP Council, says there isn’t enough time for everything she needs to do.
“But you have to make time,” she says. “I put in my own time, during lunch and after I clock out.”
Luna’s partner Sodhi agrees. The time challenge has to be reckoned with—but it’s a challenge worth solving.
“I’ve definitely made it a priority,” she says. “It was tiring devoting all that time, but I knew that I needed to do that to develop my relationships. In order to achieve any results, I knew I had to invest in time.”
“Capacity” is another word that surfaces when sponsors talk about challenges. Identifying people who can be strong sponsors and ensuring they have the tools and skills for the role is not easy. Labor bears the brunt of this barrier, in part because the unionized workforce typically has a smaller pool of leaders to draw from than management has. Many potential labor sponsors lack the consulting and facilitative skills required to mentor a team. As a result, union sponsors are in short supply, and those few become overwhelmed, with too many teams to support.
“I think that with labor, with so much work to do for our regular jobs, this is too much,” Luna explains. “So a lot of my peers didn’t want to do it. (Or) the ones who want to do it couldn’t get released because of operational needs. Patient care comes first, so operational need is a huge barrier.”
Some say successful sponsorship won’t happen until sponsors are held accountable, with their success tied to performance goals and financial compensation.
But in the meantime, many medical centers and regions are wrestling with finding other solutions to these issues. As a first step, some are revamping their training to clarify roles and responsibilities, which many sponsors — both labor and management alike — say have not been clear.
“It will be helpful for people to understand what they are supposed to do and see examples of how that’s done,” Ochoa says. “This is relatively new for some labor folks especially, and the more we can give them the tools to be a good sponsor, we need to do that.”
At the Los Angeles Medical Center, the facility’s LMP Council has made a series of changes in the last year it thinks will help shore up sponsorship. These include establishing criteria for becoming a sponsor, to make sure the right people are in the role and can model partnership and leadership behaviors; aggressively recruiting union co-leads of high-performing teams to become sponsors to increase the labor sponsor pool; and reassigning UBTs so a sponsor has no more than five teams.
Ultimately, time and commitment always will be challenges, but the potential rewards — the culture change and performance improvement work that come with high-performing teams — make the investment worthwhile. If sponsorship remains a barrier, there is a risk that teams will get discouraged.
As Luna says, “To be successful, we need successful sponsors and to build credibility with our teams. And we want to be successful.”
Deck: Helping teams do their best work
Linda J. Bodell has a simple formula for being a good sponsor of unit-based teams: Show up. Be of service. Clear a path. Bodell, a former clinical nurse specialist, spent much of her career in critical care settings where patient cases are often unstable and complex. She learned to be watchful and attentive. Today, those lessons define her as a sponsor of four teams at the Fontana Medical Center. She meets with her teams and her labor partners each month. Her personal goal is to understand what works and what doesn’t—and to get to the “why.” Bodell’s teams praise her for guiding them through facility and regional business goals, yet trusting the teams to find solutions that deliver needed results. She talked about being a sponsor with LMP senior communications consultant Anjetta McQueen.
Bodell was clinical director of Medical-Surgical Services at the time this article was written; she is now director of Clinical Care.
Q. Please share one of your best practices.
A. Show up at every team meeting, even if it’s only just one 15-minute window. It’s once a month per team. It’s essential. There is no substitute for being present. Let your teams tell you what they are currently working on. You tell them what’s going on…because they need it to complete their projects successfully. They haven’t had a bloodstream infection in 16 months? They need to hear where they are being successful.
Q. Would you describe an instance when you removed a barrier?
A year and a half ago, an RN and PCA (personal care attendant) from one of my teams asked to get a blood pressure machine that could stay in the patients' rooms. I did that—we had a department closing. I acquired a unit that could stay in one of the isolation rooms. It’s just those little things that make a difference in their work experience every day.
Q. Are there aspects of your past experience that have enhanced your sponsorship?
A. I have served on several nonprofit boards and as a volunteer, in different areas of health care and in Oman and South America, and that’s about taking a service to people, and it’s the same thing I do here as a sponsor. It’s my job to serve them so that they have everything they need to do their job the best they can. I know they care about their patients and their colleagues. They need to know that I care about them and what they do, and that it matters.
Q. Have your teams ever solved something you thought was unsolvable?
A. I would ask them! But the 4 West Med-Surg team was having a difficult time with workflows and getting to their supplies. They work where there are long hallways, where the 34 beds are arranged in a rectangular shape around the unit. This did not look like a process that could be fixed. They did the spaghetti diagram on how many steps nurses take. And the staff, together, made decisions about how to change, where they have their supplies, and how they were arranged. They worked on their workflow. Now the service scores are phenomenal.
Q. What inspires you each day in your duties as a sponsor?
A. So when you know what the goals are and what the actual plans are, and you go out and round on the department, and you can see those in living proof. It’s just exciting to see that this process really affects practice and activity at the unit level.
Words from the front line
“She really has an open door and an open heart. Linda has been a wonderful mentor. She is patient and stays calm under pressure. She knows how to lead you without just handing you the answers. She keeps you focused on what’s important.”—Letty Figueroa, RN, assistant clinical director and management co-lead, 4 East Med-Surg UBT, Fontana Medical Center
Polish Your Skills, Save the Planet
Deck: Southern California EVS teams go green with new certificate program
Cutting waste and saving money for Kaiser Permanente members and patients is good. But 350 Environmental Service workers in Southern California are taking that mission a step further by tending to Mother Earth as well.
Kaiser Permanente and two Labor Management Partnership-funded workforce development trusts are among the health care partners nationwide that are training frontline workers and managers in improved recycling, waste disposal, energy conservation and other green practices. The U.S. Department of Labor and the Healthcare Career Advancement Program, a national partnership of unions and hospitals, are leading the effort.
“‘Carbon footprint’ is a phrase that’s thrown around a lot,” says Milford “Leroy” Alaman, EVS operations manager at the Los Angeles Medical Center. “Now our staff is able to understand that when you are talking about conserving energy, water and electricity, you are talking about looking at the resources we have in our facility and holding on to just what we need instead of creating more waste for us and the planet.”
Leading change at work
Along the way, these “green teams” also are reducing operating costs, enhancing employee skills and morale, and improving patient and workplace safety.
For example, the EVS department is now using environmentally friendly microfiber mops to clean a single patient room. This has the benefit of not spreading infections between rooms and preventing lifting and straining injuries caused by wringing traditional mops and hauling buckets of water.
The department also has started a project that is reducing the cost and trouble of replacing the 500 D-cell batteries used in the hospital restrooms’ automatic towel dispensers. The traditional batteries wore out in a matter of weeks—costing about $3,000 a year to replace and adding some 6,000 batteries a year to local waste or reprocessing streams. Starting in February 2012, workers installed new rechargeable batteries. Overall, EVS' green projects, including the use of rechargeable batteries, are saving an estimated $12,000 a year.
Enhancing skills, raising sights
“I feel better having conversations with anyone…doctors, nurses, I can tell them how to be green,” says EVS attendant Jose Velasco, an SEIU UHW member and a recent graduate of a green certification course offered at West Los Angeles Community College.
The program also was piloted at KP Riverside Medical Center, where the EVS unit-based team is reaching out to others with its newfound expertise. Now an EVS member is embedded with the Operating Room UBT—with others to follow—to help tackle waste and hygiene problems there.
The SEIU UHW-West & Joint Employer Education Fund and the Ben Hudnall Memorial Trust have helped underwrite the cost of the training for Kaiser Permanente’s LMP-represented workers. Eventually, frontline workers may be able to use their certifications for higher pay and promotions as medical center “green leads,” a program that would be negotiated between KP and the unions.
But the training already is making a difference to workers as well as to KP and the community. “They have more tools, more knowledge, so they are able to catch things,” says Angel Pacheco, management co-lead of the EVS UBT at Riverside. “We talked about saving the environment for future generations.”